Science Is Art
Do mitochondria contribute to heart failure?
A grant from the American Heart Association is funding a researcher’s effort to uncover the role of mitochondria in heart failure — and confirming that his different approach to the question is worth pursuing.
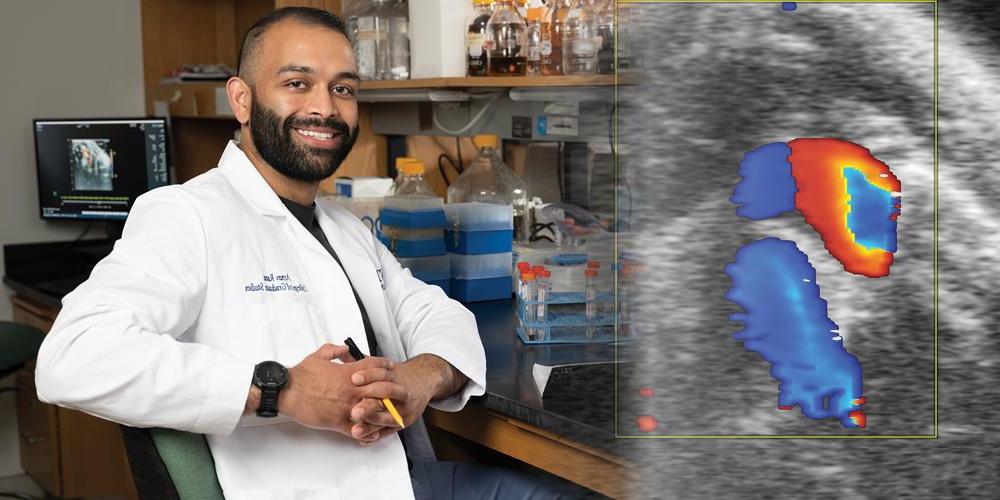
Arnav Rana, a student in his fifth year of Upstate Medical University’s MD/PhD program, is looking at how mitochondria, the so-called powerhouses of the cell, may contribute to heart disease, the No. 1 killer around the world.
Many researchers have considered mitochondria’s possible role in heart disease and heart failure. Mitochondria are organelles that generate most of the chemical energy within the cell. That energy is stored in a chemical called adenosine triphosphate, or ATP.
Most research focuses on the idea that mitochondria can become unable to produce enough ATP. That may weaken the heart so much that it stops doing its job properly. “Each beat requires a lot of energy,” Rana explains. “The thinking is when mitochondria dysfunction, they can’t produce enough energy.”
Encouraged by Upstate professors Xin Jie Chen, PhD, and David Auerbach, PhD, Rana has pursued an idea that builds on that classic thinking. Rana’s investigation looks at how certain proteins within the cell can build up over time, instead of being absorbed by the mitochondria.
Cells produce more than 1,000 proteins that must transfer into the mitochondria, but if some aren’t transferred, they can build up inside the cell cytosol, the fluid that fills much of the cell’s volume. At high enough levels, the protein buildup can affect the health of the cell and cause “non-bioenergetic stress.”
In the Chen laboratory, Arnav studies whether such non-bioenergetic stress might be a cause of heart failure and the ways in which mitochondrial stress can cause changes to the pumping ability of the heart.
To answer those questions, researchers use echocardiography, or ultrasound, of sedated mice to determine changes in heart function. Shown in the yellow box is a pulse wave doppler of the flow of blood out of the left side of the mouse heart and through the aortic valve. The red region corresponds to the flow of blood through the aorta and can be used to measure blood velocity as it exits the heart.
This article appears in the spring 2023 issue of Upstate Health magazine.